Healthcare has a high-cost, high-risk surgical instrument problem
As numerous clinical studies have shown, the majority of the tools on standard surgical trays are seldom, if ever, used in procedures. This has negative implications for patient and staff safety and hospital finances. It also increases providers’ exposure to litigation.
The problem is a vestige of a time when most surgeons were independent practitioners and hospitals competed for their business. Physician preference dictated operating room procedures, including what tools were on which trays. With changes in the business of healthcare rendering such waste untenable, there is an opportunity for a low-cost, high-reward investment in optimizing the surgical tray.
The nature of the problem
As surgery has grown less invasive and more successful in treating a wide range of conditions, the number of inpatient surgical procedures has exploded to 57 million annually in the U.S. Americans can expect to undergo seven surgeries on average in their lifetimes. Surgery departments have a considerable footprint in hospitals and deliver the majority of operating revenue and margins.
Surgery also accounts for approximately 50% of total hospital operating costs. Surgical instruments make up most of the department’s non-labor costs. Over time, the accumulation of physician preferences for specific brands and sizes of tools has caused a proliferation of surgical instruments, with some trays laden with well over 100 items. Supply costs are a particular problem in complex, high-revenue procedures such as neurosurgical, cardiovascular, and orthopedic surgeries.
When a surgical tray is unwrapped as a procedure begins, all the tools are exposed to the surgical field and must return to the sterile processing department (SPD) for reprocessing. Some instruments needlessly make the round-trip from the SPD to the OR and back hundreds of times without being used. Eventually, tools wear out and are replaced.
Most instruments stay on the tray at UChicago Medicine
- Otolaryngology – 13% of instruments used
- Plastic Surgery – 15% of instruments used
- Bariatric Surgery – 18% of instruments used
- Neurosurgery – 22% of instruments used
Beyond the unnecessary purchasing and processing costs, excessive instrumentation takes a human toll on staff. According to data from the Bureau of Labor Statistics, healthcare workers are five times as likely to get injured at work as workers overall. Sterile processing techs handle contaminated devices, work with strong chemicals, lift heavy instrument sets, and push heavy carts; they are vulnerable to injury by the very nature of the job.
According to the International Association of Healthcare Central Service Material Management, there is also almost constant pressure on SPD staff for quick turnarounds. This leads to the risk of injuries, including those caused by glove sticks. Research in 2015 found that a sharps injury generated a median cost of $747 (range $199–$1,691 per puncture). These cuts must be treated. They lead to time off for testing for diseases such as Hepatitis B & C and HIV and, for positive cases, to lengthy treatments and staff on sick leave. An 8- to 12-week course for Hepatitis B & C treatment can range from $54,000 to $95,000.
The clinical case for change
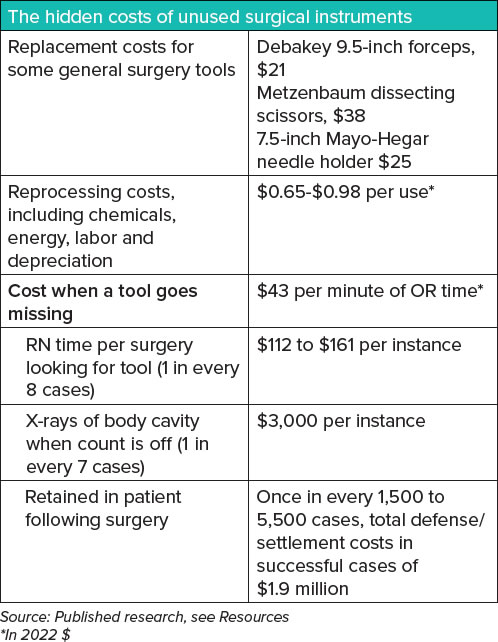
Having so many instruments increases the likelihood that some will be misplaced during surgery. When an instrument count at the conclusion of a procedure comes up short, everyone, including the anesthetized patient, has to wait for it to be accounted for. This process can take an hour or more. Few places make the term “time is money” as accurate as a surgical suite bustling with doctors, nurses, technologists, and sophisticated medical devices.
For the patient, extending the length of time on anesthesia is strongly correlated with an increased likelihood of complications, which double when operations last two or more hours and increase by 14% for every 30 minutes of additional operating time.
At a time when hospital financial margins are under stress from changes resulting from the pandemic and a generational shift to reimbursement based on value, the waste associated with unneeded surgical instruments is a significant opportunity for a low-investment, high-reward process improvement project.
Despite increased efforts to track devices and new clinical protocols, retained surgical items (RSIs) remain No. 2 on the Joint Commission’s list of Sentinel Events likely to result in serious illness or death. RSIs are believed to occur once in every 5,500 surgeries; however, this is likely an underestimate due to underreporting and the exclusion of “near miss” events. Reporting is voluntary at many institutions. Physicians commonly forgo publicizing RSI events due to fear of litigation.
Complications of retained metal objects can include perforation of the bowel, sepsis, and even death. These complications can occur early in the postoperative period or months or years later.
With the increasing use of minimally invasive surgical techniques, one can anticipate an increase in RSIs. This was the conclusion of a urological surgery team from VCU Health in Richmond, VA, which reported on a systemic review of the RSI literature in the journal Patient Safety in Surgery in 2021. “Risk factors include a limited field of view and the lack of tactile feedback for the operator, which makes it more difficult to locate a lost object and therefore increases the risk of an RSI event,” the authors wrote.
In serious cases of retained instruments, surgeons incur significant expenses for legal representation averaging approximately $30,000 in 2013 ($37,000 today), in addition to malpractice insurance ranging from $150,000 to $500,000 ($188,000-$628,000 today).
A review of one insurer’s closed claims database showed that the average indemnity payout for a claim involving a retained surgical item for hospitals and physicians was approximately $473,000 from 2007 to 2011 ($615,000 today). The average claim for cases involving permanent major damage to a patient was $2 million ($2.6 million now). The hospital incurs the added costs, estimated at as much as $76,000, for the second surgery to remove the RSI and follow-up care.

The financial case for change
Study after study of surgical tray instrumentation has found that unused tools are rampant and there are too many tray configurations. These findings also reveal significant savings opportunities.
As a baseline, researchers at the University of Chicago Medical Center discovered in 2014 that 49 surgical procedures in just four surgical specialties accounted for 237 different tray configurations. Eighty percent of instruments studied were never used.
A study at UAB Medicine in Alabama on thoracic surgeries found a reduction of “wet trays” from 2% to 0% due to fewer instruments in the autoclave. Wet or non-steam sterilized trays have water in them. All instruments in a wet tray must be re-sterilized, causing a delay in the operation start time. In addition, when a wet tray is found, all other trays running in that same autoclave load must also be re-sterilized.
After implementing a transformation to their operating rooms’ “build-to-order” process (physician preference), the UAB team removed 58,728 unnecessary instruments and eliminated all $500,000 worth of unused “sleeping” sets – weighing 29,480 pounds – from processing in the first year. Instrument assembly time decreased by 42% in neurosurgery alone, and inventory was reduced by 26%.
Conclusion
This is a simple problem. Anyone who works or visits a hospital’s instrument reprocessing center can see overloaded trays return from the OR packed with unused items. The issue of physician preference has been widely chronicled in clinical and trade journals for years. Some institutions have turned over the problem to surgeons, who are often amenable to change. More surgeons are now hospital employees, so they are more inclined to consensus building over control of which brands and makes of surgical instruments are purchased.
The issue is one of institutional will. Reflexive, ad hoc decision-making must give way to systemic change. As healthcare seeks low-cost interventions that reduce cost without substantial upfront capital and extensive IT involvement, a comprehensive system for medical instrument management is clearly needed.
Resources
Surgical Instrument Optimization: Summary of Key Studies
Cichos, KH; Hyde, CB. Optimization of Orthopedic Surgical Instrument Trays: Lean Principles to Reduce Fixed Operating Room Expenses. Journal of Arthroplasty (2019): 34:2834e-2840e
Twenty-three independent orthopedic surgical instrument trays at an academic hospital were reviewed from 2017 to 2018. Using Lean methodology, surgeons agreed upon the fewest number of instruments needed for each of the procedure trays. Instrument usage counts, cleaning times, room turnover times, tray weight, holes in tray wrapping, wet trays, and time invested to optimize each tray were tracked. The calculated total annual savings was $270,976 (20% overall cost reduction).
Dekonenko, C; Oyetunji, TA; Rentea, RM. Surgical tray reduction for cost saving in pediatric surgical cases: A qualitative systematic review. Journal of Pediatric Surgery (2020) 55(11):2435-2441.
This review of pediatric surgical tray standardization and cost-effectiveness found that on average, discontinuation of disposable instruments and standardization of equipment resulted in a removal of 40%-70% of surgical instruments per set. This yielded a cost savings of 20% (an average of $200), with no intraoperative complications or perceived safety issues.
Farrelly, JS; Clemons, C. Surgical tray optimization as a simple means to decrease perioperative costs. The Journal of Surgical Research. (2017) 220:320-326
Yale New Haven Medical evaluated instrument use across five surgical sections with the goal of cost reduction. The pediatric surgery section eliminated an average of 59.5% of instruments per tray, resulting in 45,856 fewer instruments processed per year, and nine trays eliminated from rotation. Processing time for six commonly used trays was reduced by 29%. Among all five surgical sections, annual instrument cost avoidance after tray optimization was estimated at $53,193 to $531,929.
Farrokhi, FR; Gunther, M; et al. (2015) Application of lean methodology for improved quality and efficiency in operating room instrument availability. J Healthc Qual. 37(5):277-86
Lean methodology was applied to determine instrument usage and waste, remove unnecessary instruments, and standardize trays for a given procedure. The primary outcome was a reduction in unnecessary instruments delivered to the operating room. As a secondary step, Lean analysis helped reduce the number of instruments for minimally invasive spine surgery by 70% (from 197 to 58), and setup time by 37%.
John-Baptiste, A; Sowerby, LC; et al. Comparing surgical trays with redundant instruments with trays with reduced instruments: a cost analysis. CMAJ Open. (2016): 4(3):E404-E408
This Canadian study compared the direct costs of trays containing redundant instruments to reduced trays for five otolaryngology procedures and found the cost of redundant trays was $21,806 and the cost of reduced trays was $8,803, for a 1-year cost saving of $13,000.
Kim, SH; Kim, HY. Reducing Supply Cost by Standardization of Surgical Equipment in Laparoscopic Appendectomy. Quality Management in Health Care. (2021) 30(4):259-266
A South Korean study found that the use of a standard laparoscopic appendectomy equipment set established by consensus opinions of nine board-certified surgeons decreased intraoperative costs for laparoscopic appendectomies by 25%.
Knowles, M; Gay, SS; et al. (2021) Data analysis of vascular surgery instrument trays yielded large cost and efficiency savings. J Vasc Surg. 73(6); 2144-2153
An observational study at one hospital found that less than 20% of surgical instruments were used in vascular and aortic procedures. After clinician review, 780 instruments were removed from the 13 types of vascular trays and 475 from five instances of aortic trays.
Lonner, JH; Goh, GS; et al. Minimizing Surgical Instrument Burden Increases Operating Room Efficiency and Reduces Perioperative Costs in Total Joint Arthroplasty. The Journal of Arthroplasty (2021) 36(6):1857-1863
Only 45.5% of instruments in total joint arthroplasty were used. After Lean-based optimization, 28 of 87 (32.2%) instruments were removed and the remainder could be stored in one tray. Mean set-up time decreased from 20.7 to 14.2 minutes, while 40-75 minutes were saved during the sterilization process. Average annual savings amounted to $281,298 for just four procedures.
Shaw, A; Chan, YY; et al. (2022) Streamlining surgical trays for common pediatric urology procedures: A quality improvement initiative. J Pediatr Urol;18(4):412.e1-412.e7
A team of QI, OR and sterile processing staff looked at instruments used in one of the most common procedures. Tools decreased from 146 to 65 per tray, set-up time decreased from 7.3 to 3.5 minutes, and tray weight dropped by 6 pounds.
Stockert, EM; and Langerman, A. Assessing the Magnitude and Costs of Intraoperative Inefficiencies Attributable to Surgical Instrument Trays. Journal of the American College of Surgery. (2014): 219(4):646-55
Researchers at the University of Chicago Medical Center discovered that 49 procedures in just four surgical specialties accounted for 237 different 5 tray configurations. Eighty-seven percent of instruments in otolaryngology, 85% in plastic surgery, 82% in bariatric surgery and 82% in neurosurgery were never used. An increasing number of instruments per tray was associated with decreased use and increased instrument error rate. The total cost of cleaning and repackaging an individual instrument for each case was 51 cents.
Toor, J; Bhangu, A. (2022) Optimizing the surgical instrument tray to immediately increase efficiency and lower costs in the operating room. Can J Surg 65(2)
Utilization of instruments on the major orthopedic tray at a large academic hospital was documented over 80 procedures. Results of the observations were applied to a customized mathematical model to determine the ideal tray configuration. The model produced an ideal tray size of 47 instruments, a reduction of 41 instruments from the original size of 88 instruments (47% reduction).
Van Meter, MM; Adam, RA. Costs associated with instrument sterilization in gynecologic surgery. American Journal of Obstetrics and Gynecology. (2016) 215(5):652.e1-652.e5
This single-site observational study of 28 gynecologic surgical cases (5 abdominal, 11 laparoscopic and 12 vaginal) found that surgeons used an average of 36.7 of 184 available instruments per case, for a usage rate of around 20.5%. Instrument use was correlated inversely with the number of instruments, with an average usage rate of 18.7% for trays that contained 10 instruments. Total annual per-instrument processing cost $3.19.
Weprin, SA; Meyer, D; et al. Incidence and OR team awareness of “near miss” and retained surgical sharps: a national survey on United States operating rooms. Patient Safety in Surgery (2021) 15(1):14
Researchers at Denver Health and the University of Colorado surveyed anesthesiologists, surgeons, and nurse/technologists on incidence of retained surgical instruments as well as near misses, in which instruments were not found. An average incidence of 4.4 lost instruments per 1,000 surgeries was found, with an average of 21 to 30 minutes spent searching. Adding in the use of X-rays, a lost instrument event results in up to 70 minutes of added OR time. Although previous research found that one retained surgical item occurred in every 5,500 surgeries, this study suggests incidence of one event per 3,800 surgeries.
Request More Information
If you have any questions or would like more information about SureCount’s SmartTray Surgical Instrument Management System, please use this form to send us a message.

